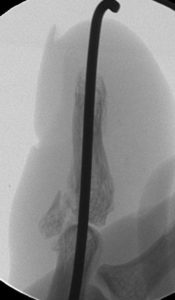
The following images represent classic signs and symptoms of Complex Regional Pain Syndrome, also known as CRPS. Historically, this has also been referred to as sympathetic reflex dystrophy or causalgia.
I have found that the most sensitive and predictive finding is a dramatic loss in function (strength or motion) of a body part that is out of proportion to the injury. Other common findings include:
- changes in skin texture on the affected area; it may appear shiny and thin
- abnormal sweating pattern in the affected area or surrounding areas
- changes in nail and hair growth patterns
- stiffness in affected joints
- problems coordinating muscle movement, with decreased ability to move the affected body part
- abnormal movement in the affected limb, most often fixed abnormal posture (called dystonia) but also tremors in or jerking of the limb.
Treatment always requires a prompt diagnosis and typically starts with therapy to improve motion and reduce discomfort. However, some evidence suggests CRPS is propagated by a compressed nerve (ie: median nerve) and surgical intervention is sometimes recommend, such as a carpal tunnel release.
The following images show patients with an open palm, and attempted closed fist, compared to the normal side.