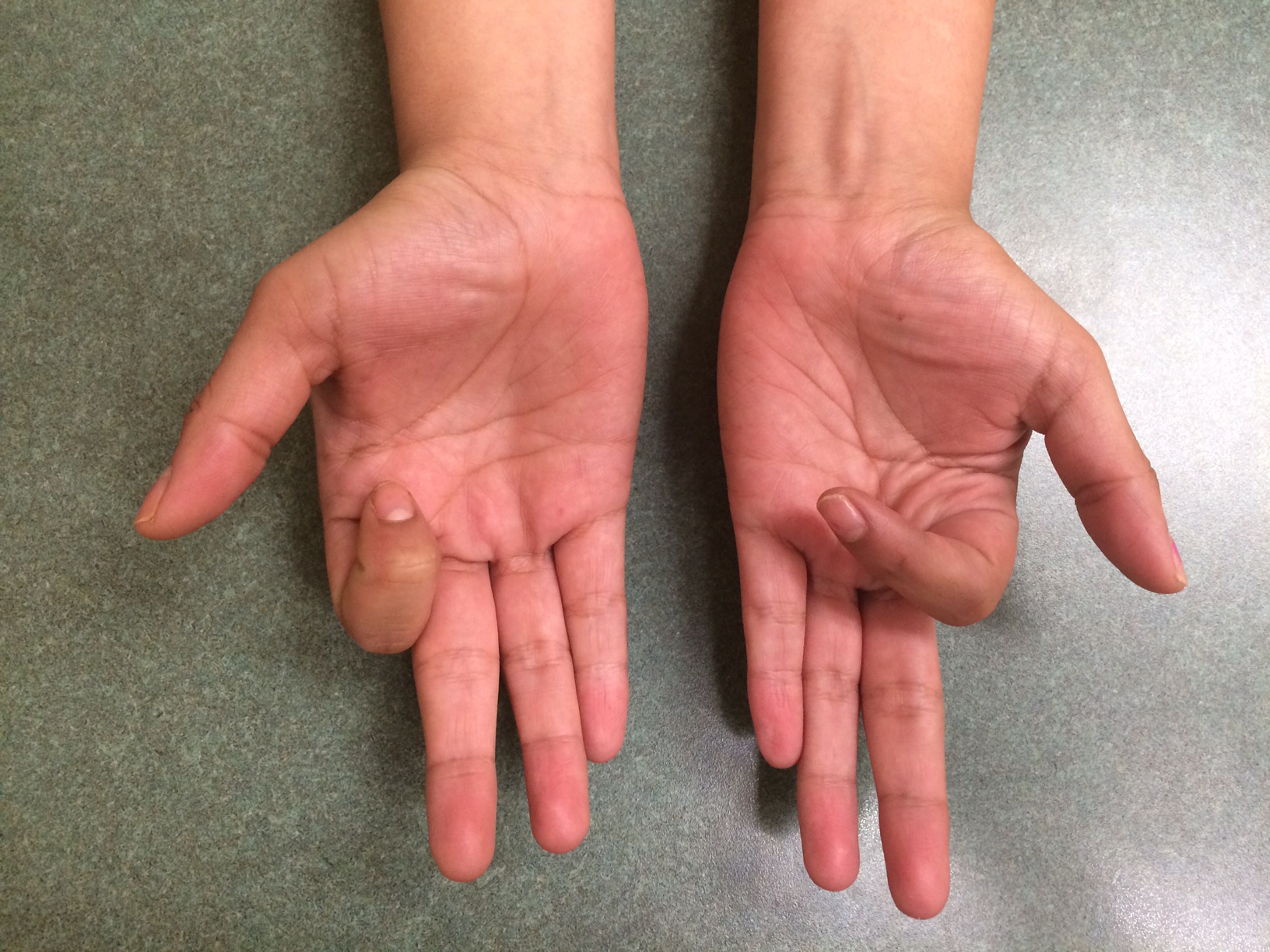
History: 39 year old gentleman came to the office after a steel beam fell on his hand, crushing his index, middle, and ring fingers. He had fractures of the proximal phalanx to all three fingers and limited motion, swelling, and pain.
Diagnosis: P1 fractures of index, middle, ring fingers



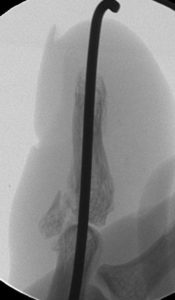
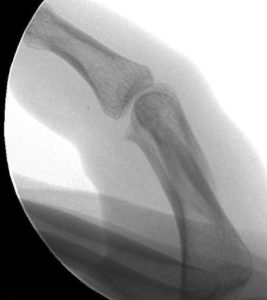
Treatment: Index and Middle fingers intramedullary screw, Ring finger pinning

Outcome: At 2.5 months he had nearly full motion and no pain. The index and middle fingers were significantly better than the ring finger in regards to motion.