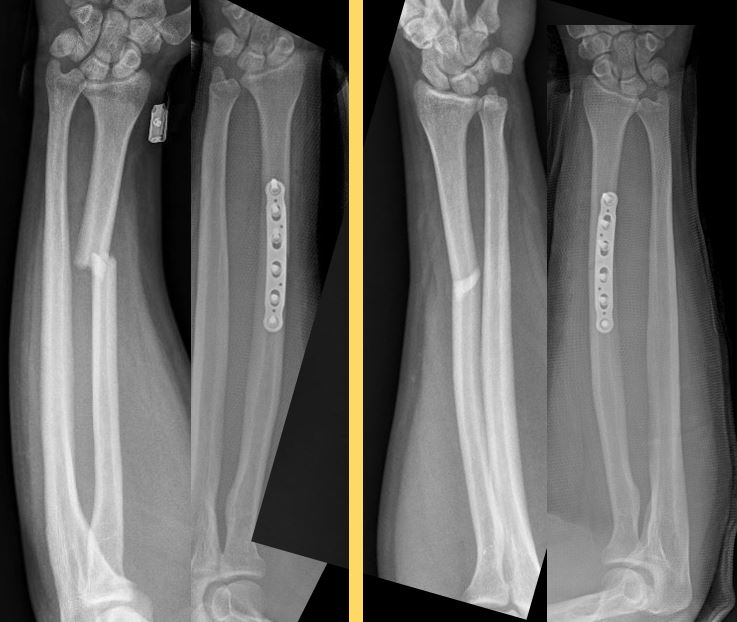
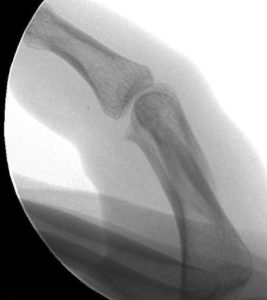
History: 79 year old gentleman sustained an elbow injury when he fell from his bicycle. He went to the emergency department where he was diagnosed as having an olecranon fracture. I met him in the emergency department to discuss surgery.
Diagnosis: Right olecranon fracture

Treatment: Olecranon open reduction and internal fixation with plates and screws


Outcome: Within 3 weeks hhe had near full motion and no pain. The scar was fully healed and nearly invisible. He was very happy with the results.